Building a Smarter Patient Statement
December 12, 2014 •Brian Watson
 Facing tight budgets and rising patient self-pay revenue, healthcare organizations of all sizes are looking for ways to more effectively collect direct patient payments - without increasing operating costs.
Facing tight budgets and rising patient self-pay revenue, healthcare organizations of all sizes are looking for ways to more effectively collect direct patient payments - without increasing operating costs.
The good news? Many of the reasons commonly cited by patients for non-payment can be solved by targeted initiatives from providers.
For example, in a recent McKinsey & Company study that examined U.S. healthcare payment trends, the top three reasons for patient non-payment - and over 80% of total responses - could be grouped into “addressable” factors, such as “Lack of financing options”, “I just received my statements”, and ”I forgot to pay or was confused about what I owe”
Smart, effective patient financial communication is often a good first step for health systems looking to efficiently meet the rising tide of self-pay receivables head-on.
Better - and more proactive - integration of financial tools and propensity-to-pay analytics, easy-to-understand patient statements and letters, and tighter control of back-end mailstream operations can help address many of the root causes of non-payment.
And that, in turn, improves revenue cycle performance: enhancing and accelerating revenue collection, reducing service calls and costs, and building upon patient satisfaction and brand preference achieved during the treatment process.
In addition, unlike many revenue cycle initiatives, upgrading patient statement quality is generally a low-impact strategy. Document design and statement processing application changes usually aren’t dependent on a large investment of staff time or financial resources.
By employing best-practice patient communication strategies, healthcare providers can collect more while using less.
Patient Communication that Improves Revenue Collection
In 2007, patient responsibility made up just 12% of total healthcare revenue. As of 2012, it had increased to 30%.
Historically, with so much revenue coming from payers, it was easy for many providers to overlook patient communication in the search for cost-containment and better revenue cycle outcomes. Not any longer.
The rising tide of self-pay revenue - and the challenges inherent in collecting from this patient segment - has many providers going back to the drawing board in pursuit of a smarter, more effective patient statement.
But what will they find when they get there? What strategies provide the greatest return-on-investment from a statement design strategy?
In the rest of this post I’ll outline four areas we focus on when we’re completing a redesign for one of our healthcare clients – culled from hundreds of statement redesigns and A/B split tests we’ve tracked over the past decade-plus.
Stress Usability
On average, patients spend five minutes reviewing each medical bill they receive. And despite the industry-wide focus on patient-friendly billing practices, many consumers still struggle to understand their statements: over 40% of consumers believe the best way to improve financial communication is to make it easier to understand.
Statement clarity was the most popular response in a recent study investigating consumer billing preferences, beating out other popular statement design options like use of color and the inclusion of educational/informational content.
Simple, clear, clean correspondence helps patients quickly understand key billing takeaways – what’s owed, for what, and by when. And proven design concepts manage eye movement and clearly highlight payment and billing support instructions.
Integrate Your Patient Financial Tools
The most efficient patient communication solutions enable providers to use all the financial tools at their disposal to more intelligently bill patients and capture payment.
For example, 80% of self-pay revenue typically comes from less than 30% of accounts. Not coincidentally, these accounts tend to be resource hogs, using a disproportionate amount of providers’ time and budgets. By recognizing where opportunities exist to reduce costs and improve collectability, providers can develop customized billing funnels that help their staff work smarter and enhance cash collections.
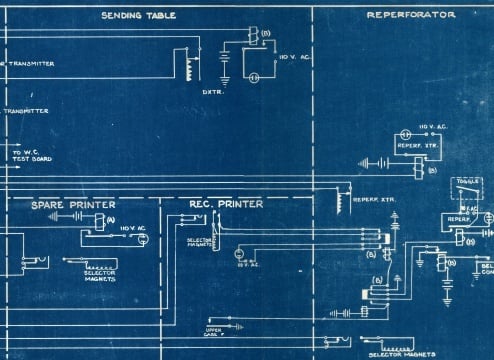
Armed with, better, faster, more efficient data management and variable print technology, providers now have the tools at their disposal to create integrated, data-infused billing that solves critical revenue cycle operational issues and bottleneck.
Many providers are now leveraging propensity-to-pay data to improve patient statement processing operations. Relying on financial analytics to help shape billing practices can reduce collections bottlenecks and increase patient satisfaction.
For example, a patient that checks-out for charity care might be presumptively enrolled in financial aid, rather than sent a statement with a balance that they might not have the means to repay. Or a patient’s credit score and financial profile may be combined with internal payment data – like the repayment rate for patients who undergo knee-replacement surgery – to programmatically suggest custom payment terms that are then integrated in a statement.
The result is smarter patient communication that achieves key financial outcomes and improves patient engagement by joining together data from across financial services.
Personalize Your Billing
Although healthcare organizations have historically maintained large repositories of patient clinical and financial data, until recently, their ability to access and use that intelligence has been relatively limited. Restricted by paper files, physical charts, and siloed software applications, key patient data often remained disconnected and under-utilized.
Recent advances in healthcare information management are quickly evolving the traditional model, however. Spurred by widespread adoption of Electronic Medical Records and new health information systems that can quickly and efficiently integrate data from both internal silos and external sources, today’s hospitals, health systems, and medical groups have an unprecedented level of actionable patient data at their disposal.
From a patient design standpoint, the ease and speed with which patient data can be stored, retrieved, and analyzed has several positive implications. For one, personalization of patient communication enhances engagement and helps providers reach financial objectives. A specialized consultation with a skilled physician or nurse practitioner will yield far more detailed, comprehensive results than a patient is likely to receive reading a generic WebMD article.
Similarly, a statement that is personalized with lifetime transaction data or specialized financial analytics is more likely to resonate - reducing the chance that a Spanish-speaking patient receives a bill in English, for example. Or that the balance due reflected on patient’s paper statement isn’t the same figure that is quoted in an online payment application.
A personalized approach not only reduces monthly statement volume, it also enables your patient financial staff to use their time most productively.
Get Updates
Featured Articles
Categories
- Charity Care Management (1)
- Compliance (2)
- Customer Service (8)
- Digital Front Door (1)
- Direct Mail (6)
- eBilling (1)
- EBPP (34)
- ESL Statement (2)
- eStatement (1)
- Healthcare Channel Partner Billing (1)
- IVR (3)
- Mobile Payment (11)
- Online Billing and Payment (6)
- Online Patient Payment (17)
- Outsource Print Management (4)
- Paperless Billing (4)
- Patient Engagement (2)
- Patient Friendly Billing (21)
- Print and Mail (7)
- QR Codes (1)
- Quick Pay (7)
- Security (1)
- Self-Pay Patients (9)
- Self-Pay Revenue (4)
- Statement Design (32)
- Statement Print and Mail (1)
- Statement Printing and Mailing (28)
- Statement Processing (36)
- TransPromo (1)
- Up-Front Billing (1)